Understanding Spinal Nerve Function and VA Claims for Back-Related Conditions
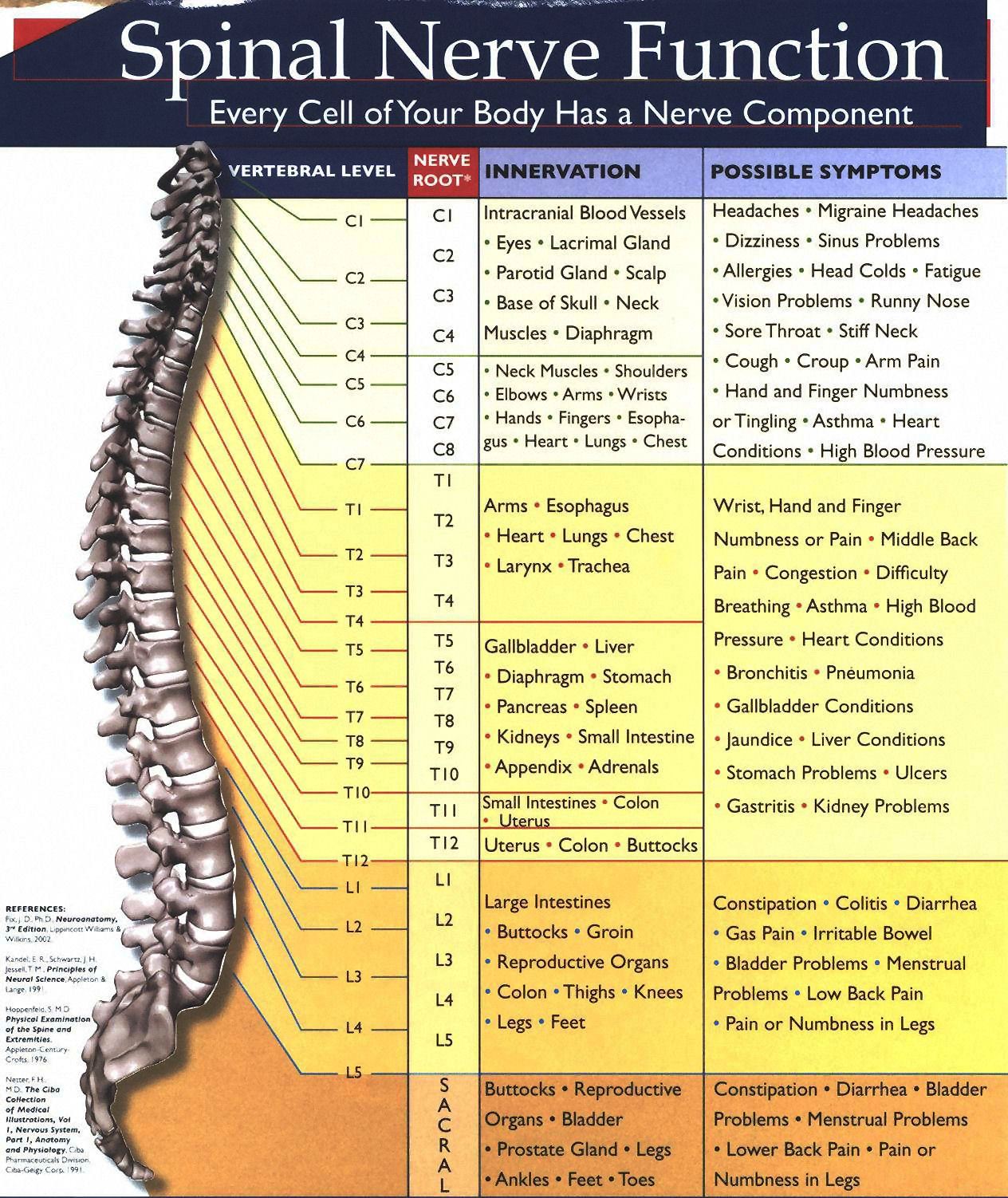
The graphic presented here illustrates spinal nerve function across the different regions of the spine: the cervical spine (C1–C7), the thoracic spine (T1–T12), the lumbar spine (L1–L5), and finally, the sacrum. This anatomical reference is crucial when examining how spinal issues may relate to specific symptoms and conditions that are potentially eligible for VA disability benefits.
As explained by a VeteransBenefitsHub.com contributor, they have undergone an anterior discectomy and fusion at cervical levels C3–C4 and C4–C5. These joints no longer move independently; they function as a single unit due to the fusion. Additionally, the contributor reports a significant herniated disc at L5–S1, where the lumbar spine meets the sacrum.
Symptoms Linked to Spinal Regions
Each region of the spine corresponds to different organs and bodily functions. For instance, issues at the T1 vertebra (part of the thoracic spine) may affect the heart, lungs, thymus, bronchial tubes, trachea, chest, breast, pleura, gallbladder, arms, shoulders, and upper back. Associated symptoms could include:
- Heart conditions
- Asthma
- Bronchitis
- Indigestion
- Difficulty swallowing
- Nausea
- Headaches
- Fatigue
- Chronic coughing
- Shortness of breath
- Bloating after eating
Veterans experiencing these symptoms may want to consider whether a spinal condition is affecting a secondary organ system. This becomes particularly relevant when pursuing a secondary service connection claim.
Filing a Secondary Service Connection Claim
To strengthen a claim, it’s essential to have a medical opinion, known as a “nexus,” linking the secondary condition to the already service-connected spinal issue. For example, if a veteran has a service-connected low back condition rated at 10%, and they also have asthma related to spinal nerve compression at T1, a medical professional must provide documentation connecting the two.
Understanding VA Ratings Criteria
According to 38 CFR § 4.71a, the VA evaluates spinal conditions based on range of motion, functional loss, and pain. The Compensation and Pension (C&P) exam will involve physical tests to assess flexion, extension, lateral flexion, and rotation.
These are measured using a goniometer—a plastic protractor-like tool. If a C&P examiner does not use this device and relies solely on visual estimation, the exam may be considered inadequate. Veterans should advocate for proper measurement techniques to ensure an accurate assessment.
Rating Examples
- 10%: Common initial or “lowball” rating.
- 20%: Slightly more significant, but still frequently assigned.
- 40%: Typically awarded for severe range-of-motion limitations and chronic pain.
Veterans aiming for an increase must fall within the higher rating criteria. For example, limited forward flexion to just 5 degrees—where pain begins—should be documented. Veterans are reminded not to push through pain to satisfy the examiner. The C&P examiner is not a treating physician, and their role is solely to evaluate the disability for rating purposes.
Resources for Navigating VA Claims
Veterans are encouraged to reference the Code of Federal Regulations (38 CFR), specifically the schedule of ratings for the musculoskeletal system. Additionally, the M21-1 Adjudication Manual can provide insight into how VA adjudicators review claims. Requesting a copy of one’s claims file is also advisable to understand the evidence already on record.
